The Care Team
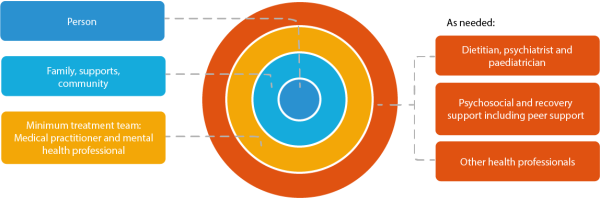
Eating disorders are complex and multifaceted. While the minimum treatment team is a medical practitioner and a mental health professional, input from practitioners from a range of disciplines is often necessary for comprehensive care. Family and supports are integral to the care team.
The care team consists of the person experiencing an eating disorder and all people who will be involved in providing care, support, and/or treatment. The treatment team consists of the professionals within the care team who are providing treatment for a person experiencing an eating disorder.
Click here to view.
As shown in the figure above, at the centre of any care team is the person experiencing an eating disorder, and their family, supports and community. Treatment plans should always be developed within a person-centred, family and culture-sensitive and recovery-oriented framework (NEDC, 2018) and thus information and decision making is shared between all members of the care team, including the person experiencing an eating disorder, their families, and supports.
How the treatment team works
As portrayed in the outer circles of the diagram above, a treatment team may involve other professions, depending on the needs of the person experiencing an eating disorder. Dietitians, psychiatrists and paediatricians can often be an integral part of the multidisciplinary team, with other professionals as needed (e.g., peer support workers, exercise physiologists). This will be determined by the type of eating disorder, the type and severity of symptoms, the treatment setting, and the need to meet the person’s psychological, physical, nutritional, and psychosocial needs.
A treatment team’s capacity to work collaboratively in assessment, treatment planning, and treatment review is essential for safe and effective treatment. With the different components of treatment working collaboratively together, progress in one domain (such as physical or psychological) will enable and support progress in each of the other domains.
When working with a person experiencing an eating disorder, the treatment team should be respectful of and respond to the specific needs, preferences, and values of the person throughout the co-development of a treatment plan. Sometimes however, the eating disorder may compromise a person’s capacity to make decisions in alignment with their long-term goals. In situations of deteriorating physical or mental health that require immediate intervention, the treatment team should strive to plan and implement treatment in collaboration with families and supports that is consistent with the person’s expressed wishes.
Minimum treatment team
At a minimum, a treatment team in the community (as opposed to those in a hospital setting), should be made up of a medical practitioner and a mental health professional. In the case of self-help or brief digital therapies, the person may not have a multidisciplinary team, but should be connected to medical care to ensure safety.
Medical practitioner
A medical practitioner could be a GP, paediatrician, physician, psychiatrist, or other qualified medical practitioner that is able to provide treatment and management of the physical symptoms of the eating disorder. This includes medical monitoring and treatment of medical complications associated with eating disorders, and sometimes prescribing medications.
Mental health professional
A mental health professional is an umbrella term for those professions that can provide psychological support and evidence-based psychological treatment for people experiencing an eating disorder. These professions include psychologists, social workers, occupational therapists, psychiatrists, counsellors, mental health nurses, nurse practitioners, and psychotherapists. A mental health professional is an essential part of the treatment team and will work collaboratively with a medical practitioner to provide holistic treatment and support for the person living with an eating disorder and their family and supports. A mental health professional may specialise in providing treatment for different types of eating disorders, or sometimes just one type of eating disorder depending on their training and experience. The type of treatment provided will vary depending on the type of eating disorder the person is experiencing. In addition, eating disorder mental health professionals can:
- Identify, assess, and diagnose eating disorders and other mental health problems
- Develop and implement an evidence-based treatment plan
- Provide psychoeducation and support for the individual, family and supports
- Identify the need for referral to other professionals and levels of treatment within the stepped system of care
Other professionals

Click below to learn more about the role of other professionals that may be involved in the treatment team. These professions may fill the role as the key medical practitioner (for example, a general practitioner), as the mental health treatment provider, or as a member of the broader treatment team including allied health.
The inclusion of these professions in the treatment team will be determined by the needs of the person experiencing an eating disorder.
General practitioners
GPs are often the first point of contact for a person experiencing disordered eating or living with an eating disorder and their families and supports. GPs will complete a comprehensive assessment and referral for mental health treatment providing crucial access to evidence-based care.
GPs can:
- Complete a comprehensive eating disorder assessment
- Provide additional information about the eating disorder
- Refer to a mental health professional for focused eating disorder assessment, diagnosis, and treatment
- Refer to other professions as members of the multidisciplinary treatment team
- Conduct medical monitoring and provide treatment for the medical complications associated with eating disorders
- Coordinate the treatment team across the course of treatment
- Provide recovery support including monitoring for relapse and rereferring to other professionals if required
NOTE: Your GP may also be a provider of Focused Psychological Therapies and have completed training in evidence-based psychological treatment for eating disorders. This would provide them with the knowledge and experience to provide first line psychological therapy in addition to managing the medical consequence of the eating disorder.
Dietitians
Dietitians are tertiary educated professionals with the qualifications and skills to provide expert nutrition and dietary advice. Dietitians often play a significant role in the treatment of eating disorders through providing specialised nutrition advice and support.
Dietitians can:
- Complete a nutrition assessment and conduct ongoing monitoring and evaluation
- Provide nutrition intervention including structure, education and support to encourage regular and normalised nutritional intake and eating behaviours
- Provide nutrition support for specific needs (e.g. pregnancy, diabetes, gastrointestinal disorders)
Psychiatrists
Psychiatrists are medical professionals who specialises in diagnosis and treatment of mental, emotional, and behavioural disorders. All psychiatrists will have completed medical training and additional supervised psychiatric practice.
Psychiatrists can:
- Complete a comprehensive assessment for an eating disorder and other mental health disorders
- Develop and review treatment plans including eating disorder management plans and mental health care plans under the Medicare - Benefits Schedule
- Provide medical care and treatment for the eating disorder and complications associated with the eating disorder
- Refer to other professionals required for treatment
- Prescribe medications as required
- Provide focused psychological treatment for eating disorders and other mental health disorders
Paediatricians
Paediatricians are medical professionals specialising in the physical, mental, and behavioural development of children and adolescents. Paediatricians are often involved in the treatment of children and adolescents living with an eating disorder.
Paediatricians can:
- Complete a comprehensive assessment and provide a diagnosis
- Develop and review treatment plans including eating disorder management plans under the Medicare Benefits Schedule (MBS)
- Provide medical care and treatment for the eating disorder and complications associated with the eating disorder
- Provide specialist information on growth and development in relation to the eating disorder
- Refer to other professions required for treatment
- Prescribe medication as required
Psychologists
Psychologists are tertiary qualified mental health professionals and are commonly involved in the treatment of eating disorders and co-occurring mental health disorders. Central to the role of psychologists is assessment, formulation, diagnosis, and treatment of mental health, behavioural, and emotional disorders across age groups. Psychologists can provide support and treatment for people experiencing co-occurring mental health disorders and related difficulties, including (but not limited to) psychiatric risk, trauma, and developmental disorders as well as conducting assessments of learning and cognition.
Social workers
Social workers can be involved in the treatment team as a mental health professional or as an allied health practitioner. Social workers focus on a person’s social systems and the way these systems can be supported and changed to meet their needs. This can include a person’s individual stressors, their family, community, and wider social system. Social work interventions aim to assess and meet a person’s psychological and practical needs through counselling, education and advocacy. Social workers can be found in private practice, hospitals and health services, and community organisations.
Occupational therapists
Occupational therapists (OTs) can be involved in the treatment team as a mental health professional or as an allied health practitioner. OTs assess the impact of an eating disorder on a person’s daily life, which includes their ability to engage in meaningful and important activities such as self-care, school, work, leisure, and social interactions. Engagement in these activities can enhance or re-establish important life skills and roles, supporting the development of a strong and supportive social network. OTs can be found in private practice, hospitals and health services, and community organisations.
Counsellors and psychotherapists
Counsellors and psychotherapists are trained professional that works with people and their families and supports to address personal and mental health problems. Counsellors and psychotherapists work in a range of settings, including family services, non-government organisations, community-based health agencies, and some work in private practice.
Nurses
Nurses form an important part of the multidisciplinary treatment team as a provider of medical and/or mental health care. Nurses can obtain further qualifications as a mental health nurse or nurse practitioner which allows them to fulfil other roles outside of those related to the physical care of someone living with an eating disorder including in the provision of mental health assessments and treatment. Nurses may have roles in providing medical and/or mental health care during hospitalisation or in community treatment settings, both as part of outpatient or inpatient programs.
Other health professionals
Other health professionals such as exercise physiologists, physiotherapists, and speech pathologists may be involved in the assessment and management of eating disorder comorbidities.
Other medical specialists
Other medical specialists such as endocrinologists, gastroenterologists, cardiologists, nephrologists, and physicians may be involved in monitoring and managing medical consequences of eating disorders or comorbid conditions.
Psychosocial and recovery support including peer support

Psychosocial and recovery support services and programs are generally delivered by community-based organisations, with funding from the Commonwealth and State and Territory governments, as well as through lived experience organisations and the peer support workforce (a part of the Lived Experience workforce). Psychosocial support can support the broader psychological and social needs of the person experiencing or at risk of an eating disorder and their family/supports and community. Recovery support can assist a person experiencing an eating disorder to engage with or sustain recovery or improved quality of life and assist family/supports and community in their caring role.
Peer support work is a form of psychosocial and recovery support that involves connecting with others who have had similar experiences or challenges. Peer support work can take many forms, including one-on-one conversations, support groups, and online forums. It can be delivered by people with lived experience of an eating disorder to people experiencing an eating disorder, or by people with lived experience of caring for someone with an eating disorder to other people in a caring role.
Choosing a therapist
When choosing a mental health professional, it is important to remember that the relationship you have with your treating clinician is vital. At the centre of a good therapeutic relationship lies:
- Understanding – your clinician understands your experience of living with an eating disorder and your emotions and feelings, and you understand their role in the treatment and recovery process
- Trust – you trust your therapist and your therapist trusts you; give time for trust to develop
- Rapport – you can talk openly and be heard without judgement
- Collaboration – you and your therapist work as a team, developing mutual understanding, setting goals and following through on objectives
- Education– your clinician provides you with the information you need to understand the eating disorder and other difficulties you may be facing, and provides a comprehensive outline of the planned treatment and possible multidisciplinary care team support
We encourage people to ask the questions in this Consumer checklist before starting their treatment journey.

